
In Part 1 (2018) of this series, I described why a physician without diabetes (me) would wear a continuous glucose monitor (CGM): Why I decided to wear a continuous glucose monitor as a non-diabetic physician
I followed up with a Part 2, which this post updates based on the change in technology.
Disclaimer/Caveats

- I don’t live with diabetes or prediabetes. If you as a reader has experience to impart, teach me. I want to learn.
- I am a non-obese human who is fat-metabolism adapted, eating a real-food, low carbohydrate, diet, absent any industrialized bean and seed oils.
- I’m not going to mention the manufacturer of the device used, consistent with my independence, freedom from conflict, and no endorsement of products or services statements
Acquiring the device
In the United States, a physician order is required to purchase the device, even if using personal funds (which I did – no health care premium dollars were used to subsidize this experiment). In Canada, this is not the case, as physician colleagues there have been able to purchase the device over the counter. The manufacturer will assist by providing the wording of the order that the physician needs to write to allow access at a retail pharmacy.
The device was initially sold as two devices, a reader and a sensor. The reader is still available, but no longer necessary as the sensor now communicates directly with an iPhone via NFC.
Installation and Operation

The system is ingeniously put together. I assume it has to be for something as sensitive as diabetes management. The sensor comes with an applicator that pushes a close to 1″ needle into your upper arm, in my case my triceps muscle. The sensor will stay there 24/7 for 14 days. It is safe to bathe, swim, or workout with the sensor in place. I did all of these things, sometimes quite intensively, and the sensor worked for the entire time.
I have now had incidents of sensor loss either due to scraping my arm against a hard object like a door or another person. I tend to walk in a protection stance when I am wearing the device.
I don’t mind being asked what it is wherever I go. It’s a good test to see how much the population knows about this technology (not very much at all) or the experience of having diabetes. Currently 88% of the US population does not have diabetes. In a future iteration, it might be nice to have a flesh colored sensor that doesn’t stand out as much. In my situation, though, I’ve loved every conversation started with the device.
True and thank you. Today asked "You wear a #CGM and are not diabetic?" And I said, correct, I want to understand more of what it is like to be one (and I never truly will) Always #WorkingToBeAlly ✌️🕊🏳️🌈
— Ted Eytan, MD, MS, MPH (@tedeytan) May 1, 2019
This brand of meter arrives calibrated; it will be 1 hour before you get your first reading, and then readings will occur every 15 minutes if you don’t do anything. You can acquire readings more frequently if you’d like, up to 1 a minute.
The sensor will store 8 hours of readings, which means you need to scan the sensor at least that often, or you will lose data. This experience, of being tethered to a device like this, was a good experience for me to have. Why? Because all I needed to do was wand the sensor every 8 hours. This is a fraction of the work that a person living with diabetes must do to maintain their health and prevent life threatening complications.
When a reading is scanned, there’s an option to include information about food (carbohydrate counts), exercise, or other custom notes. The device keeps track of pre-meal and post-prandial readings, which is nice.
The Interface and the Software
The iPhone app has a fairly simple interface and will do some basic trending.
There are two official software options to analyze the data: A desktop software program, and web-based one. The desktop software only works with the older reader-version of the kit. I now exclusively use the web-based version of the software. The phone automatically uploads all readings to the manufacturer’s cloud for analysis.
The iOS software is more elegant in terms of setup and manages a few issues that I noticed with the desktop software’s assumptions about target glucose level and carbs per meal.
The interesting thing is, there’s really no reference on what a glucose level should be for a non-diabetic person on a 24/7 basis. There’s this guidance from Richard Bernstein, MD:
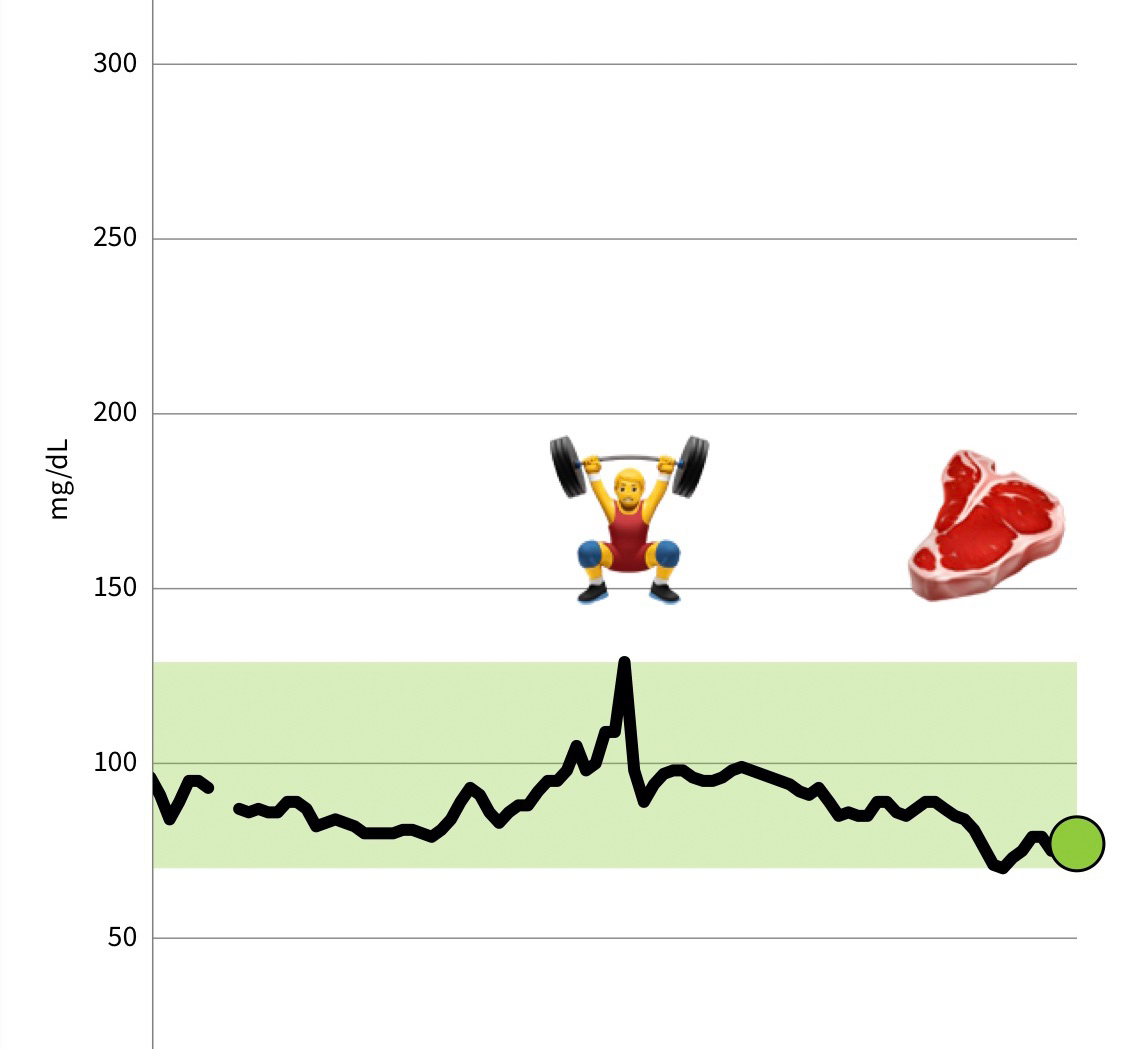
“Keep Your Glucose Levels Tightly Controlled Between 70 and 100 mg/dl all day long, everyday… or else you will pay the consequences.”Source
I am managing to do that quite well, and where I used to do sophisticated analysis with the raw data, I find I can tell stories from the data that’s presented day by day, like this one:
Isn’t it amazing how the liver can shovel glucose into the tissues at high speed, on demand, even though none (glucose) has been eaten (it is):

New Insights, Much Wonderment

To be able to see how your body regulates glucose is really a thing of wonder that we haven’t been able to do until now. I am in awe of what the body can do, and do it well. At the same time, I am also in awe of the impact of the body failing to do what it needs to do well, and how serious a situation that can be, especially if worsened by the nutrition/advice given by the health profession(s).
The photo to the right is one of my first measurements, from the old (reader) kit
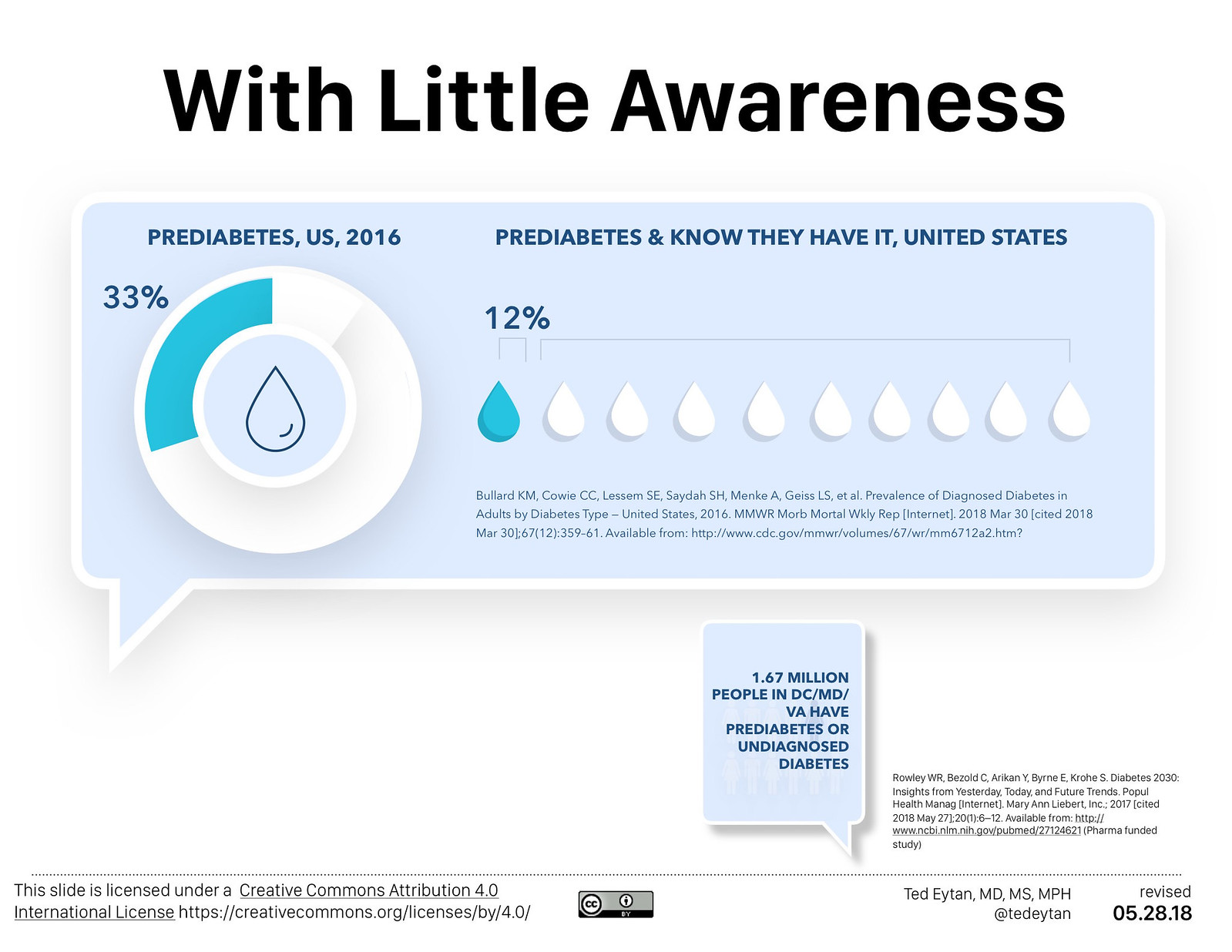
88% of people with prediabetes don’t know it
I understand that things like ECGs are being integrated into the wearable world, but really, they don’t hold a candle to the impact of understanding one of the most important risk factors for health and life. This is especially true in a country where the majority (88%) of people with pre-diabetes don’t know they have it, and are therefore very likely to progress to fulminant diabetes.
This paper shows a graphic of the incubation period – up to 10 years before glucose intolerance shows in normal screening

The future
The old reader has now been integrated into our mobile phone. I’m sure the engineers in Cupertino will be able to tell us what will happen to the sensor… 🙂
Should every human wear a continuous glucose monitor? I’m not sure. Should they wear it episodically to see how they’re doing? Maybe. I previously posted on a paper describing today’s use of CGM in medical practice, and its gaps in not recognizing this device as a part of a diabetes pre-emption strategy.
Will these be integrated into wearable devices eventually anyway? Probably.
I’ve since purchased many more sensors and there are now many parts to this story, which you can access here
My Why (am I doing this)?
I get asked this a lot. Read:
- Part 1: Why I decided to wear a continuous glucose monitor as a non-diabetic physician
- Part 10: Wearing a Continuous Glucose Monitor as a non-diabetic Physician: Impact of a (mostly) meat diet; Learning about the lives of people with diabetes
Feel free to ask questions or add comments in the comments.
My disclosures
I have none. You may see a full accounting on this page.