
I thought about making this post accessible to a lay audience, however, in the interest of expediency, I’ll just speak in scientific language. Feel free to ask questions in the comments.
This paper is a study of 100+ patients in China, with a subset of 16 patients with confirmed coronavirus illness who were tested using two different tests:
- A “molecular” or really “viral” test – this is the kind of test being used today. It detects the genetic material of viruses from the part of the body sampled from. Samples are obtained via swab from the nose, throat, lungs, or anus (by the researchers). Today, most samples are obtained via the nose (back of throat).
- A “serology” or really “antibody” test – this is not the kind of test being used today (yet). It looks for the body’s reaction to the virus – antibodies. This is important because this is the body’s memory of a pathogen. Typically, antibodies will be available for a time after the pathogen is gone. Meaning, we can tell if someone has had an infection in the past.
We can test for antibodies
This is a good finding. The coronavirus is indeed immunogenic, and very specifically so.
- There’s a rise in IgM antibodies in the beginning of an infection (as tested at day 10 of medical treatments for the 16 patients).
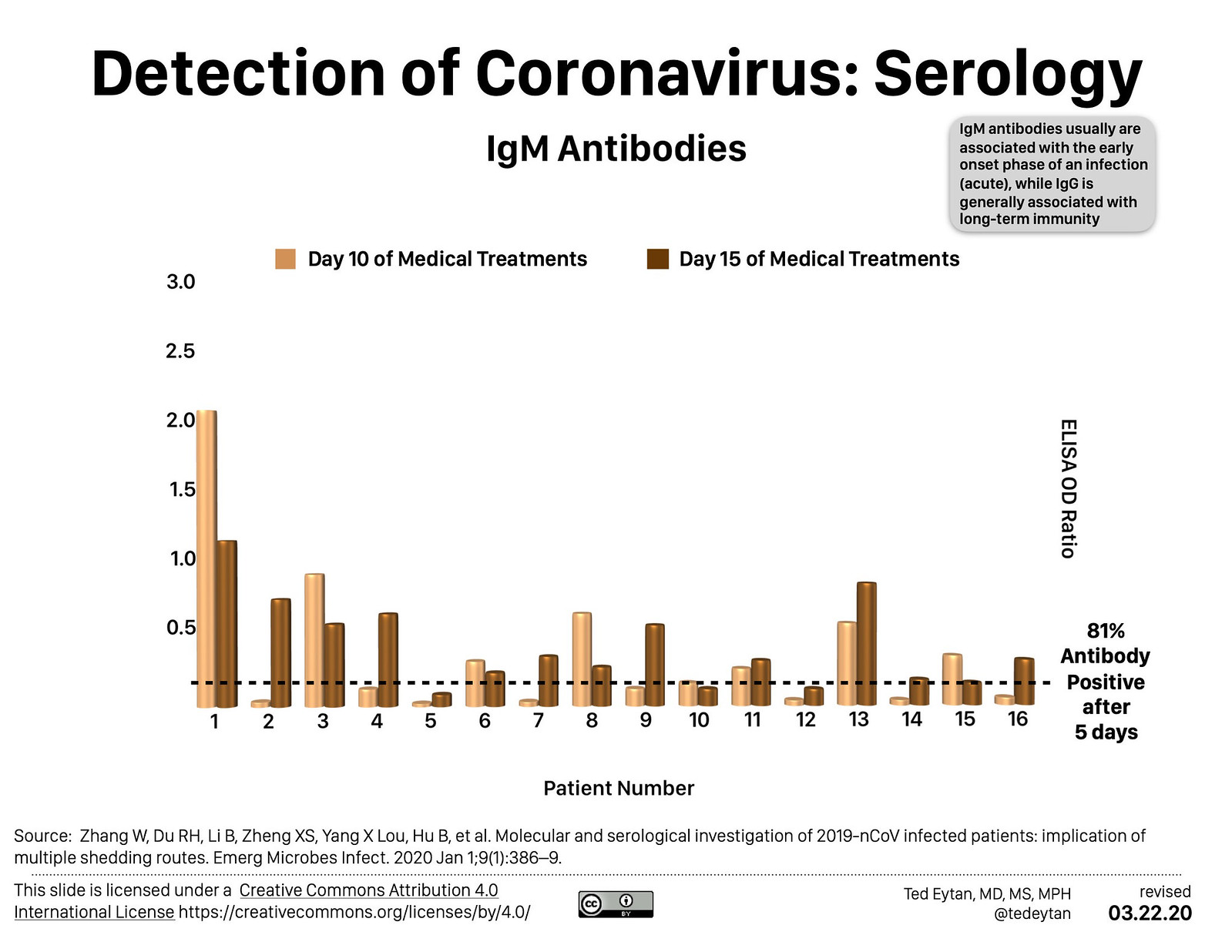
- There’s a rise in IgG antibodies, the most important ones for long lasting immunity, to the point that 100% of the 16 patients tested positive at day 15 of medical treatments.

This type of test (ELISA) is the kind that was used in the early years of HIV/AIDS. From a complexity perspective, it’s an easier test to do than the viral test. My understanding is that this type of test could be packaged in a self-contained unit. It does require blood, though.
The current test has limitations
As the study shows, what seems to happen is that the virus initially tests positive in the upper respiratory tract, and then tests negative there, and then positive in the intestinal tract (anus). This may indicate that testing only from the nose/throat may cause an incorrect intepretation that the infection is cleared. This is bad because it would cause more people to be infected.
We are flying blind today, how to fly with instruments
There is now more commentary (including from our government) that both tests have a place. An antibody/immunity test can discern people who have had the infection in the past, even if they didn’t know it. A molecular/virus test can show which of those people are actively infected.
Using both of these tests, as the authors (and several other writers) describe, may be a key to isolating the right people instead of all people.
We show that the current strategy for the detection of viral RNA in oral swabs used for 2019-nCoV diagnosis is not perfect. The virus may be present in anal swabs or blood of patients when oral swabs detection negative. In SARS-CoV and MERS-CoV infected patients, intestinal infection was observed at later stages of infection [7–9]. However, patients infected with 2019-nCoV may harbour the virus in the intestine at the early or late stage of disease. It is also worth to note none of the patients with viremia blood had positive swabs. These patients would likely be considered as 2019-nCoV negative through routine surveillance, and thus pose a threat to other people. In contrast, we found viral antibodies in near all patients, indicating serology should be considered for 2019-nCoV epidemiology. A possible shift from oral positive during early infection to anal swab positive during late infection can be observed. This observation implied that we cannot dis- charge a patient purely based on oral swabs negative, who may still shed the virus by oral–fecal route. Above all, we strongly suggest using viral IgM and IgG serological test to confirm an infection, considering the unreliable results from oral swabs detection. In summary, we provide a cautionary warning that 2019-nCoV may be transmitted through multiple routes. Both molecular and serological tests are needed to definitively confirm a virus carrier.Zhang W, Du R-H, Li B, Zheng X-S, Yang X-L, Hu B, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect [Internet]. 2020 Jan 1;9(1):386–9. Available from: https://www.tandfonline.com/doi/full/10.1080/22221751.2020.1729071
Reference
Zhang W, Du R-H, Li B, Zheng X-S, Yang X-L, Hu B, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect [Internet]. 2020 Jan 1;9(1):386–9. Available from: https://www.tandfonline.com/doi/full/10.1080/22221751.2020.1729071
Additional, relevant articles
- Rapidly identifying workers who are immune to COVID-19 and virus-free is a priority for restarting the economy | VOX, CEPR Policy Portal
- What Is The Coronavirus ‘Antibody Test’ – And How Will It Work? | HuffPost UK Life
- See: New blood tests for antibodies could show true scale of coronavirus pandemic | Science | AAAS