I was recently asked about the influences on physicians in the counseling and advocating of nutritional approaches.
People believe physicians have complete autonomy in fitting nutritional guidance to the needs of the patient. So, for example, if they wish to support approaches such as carbohydrate restriction for people with insulin resistance, they are free to do so.
The situation is not as patient-focused as the people we serve would hope.
First, a recent example:
The References Cited @AFPJournal’s “Diets for Health” Don’t Support the Content
American Family Physician (@AFPJournal) is the peer reviewed journal of my specialty society, the American Academy of Family Physicians (@AAFP). They just published a piece called “Diets for Health,” which I wrote some initial thoughts on last week.
This claim in in the paper struck me as unconventional:
Dietary fats affect serum cholesterol levels and CAD risk differently. Compared with saturated fats, increasing mono- or polyunsaturated fats decreases the risk of CAD,(39) although saturated fats found in plants may have a more beneficial effect on lipid levels.41,42American Academy of Family Physicians. A, Schneiderhan J, Zick SM. American family physician. Am Fam Physician [Internet]. American Academy of Family Physicians; 2018 Jun 1 [cited 2018 Jun 4];97(11):721–8. Available from: https://www.aafp.org/afp/2018/0601/p721.html
So I pulled references 39, 41, and 42
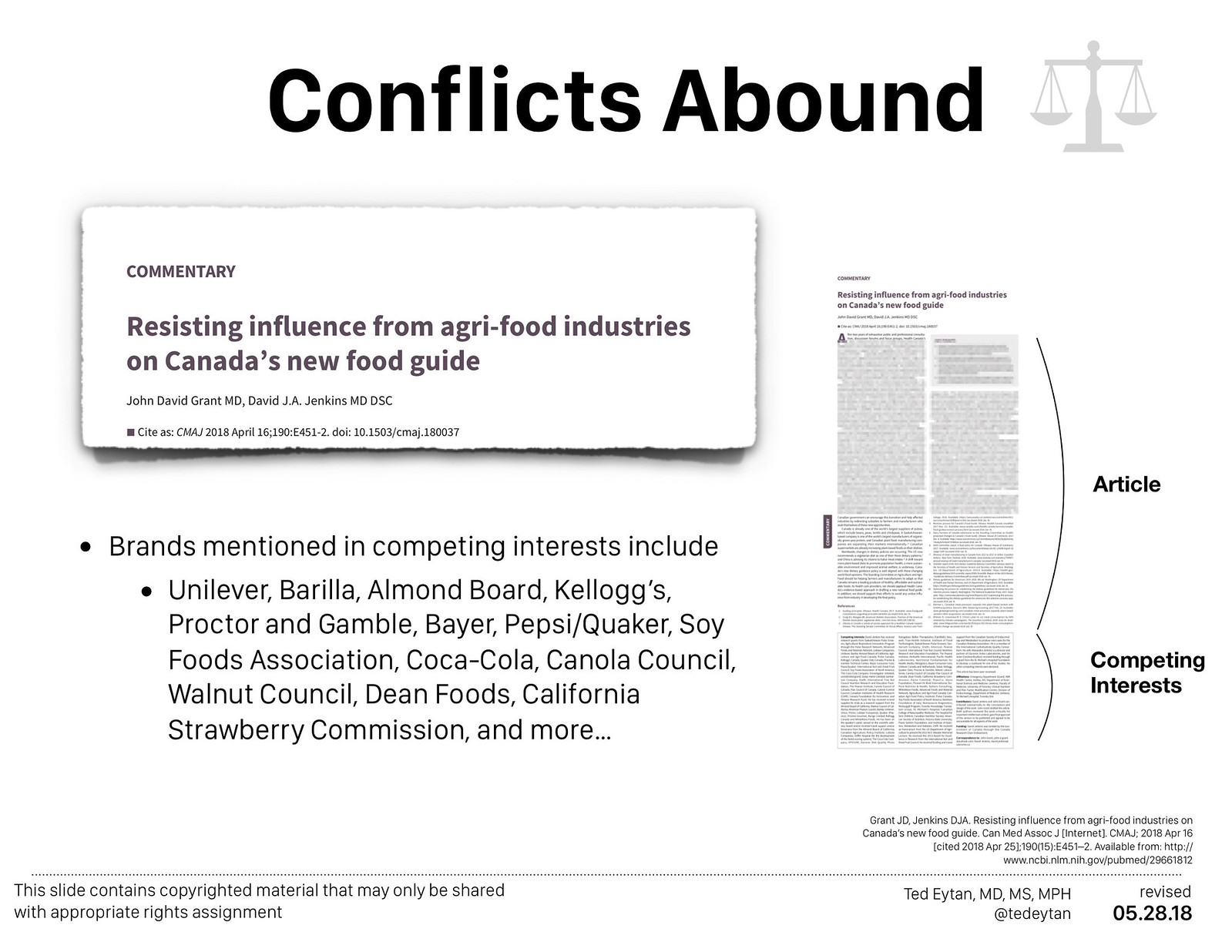
- Reference 39: Part of a series of papers written by a team at Harvard University School of Public Health, which is an epidemiological review of two large data sets. A review of the commentary on this series raises serious questions about conflicts of interest as well as the robustness of the conclusions.
- What’s not cited is the PURE study, which is more recent and doesn’t appear to suffer from the conflicts mentioned for this reference (see: Just Watched (again): Andrew Mente, PhD – “Current advice to limit total fat to less than 30%E and saturated fat to less than 10%E are not supported by this global study”)
- Reference 41: “Footnote 2: Supported by the United Soybean Board, St Louis, MO” Putting that aside, this paper, published almost 10 years ago, is really focused on the replacement of trans fatty acids with certain saturated fats found in industrial oils, the ones produced by the study sponsor (see “Footnote 2”). The paper also references the study group of Reference 39 as a basis for promoting polyunsaturated fatty acids. Let’s hold that thought and go on to…
- Reference 42: Directly contradicts what is said in the statement above altogether:
Given the complexity of the above lipid and lipoprotein esponses to ingestion of saturated fats, and given the variable contents and patterns of individual saturated fatty acids in dif- ferent food sources of saturated fats, there is no simple means of estimating the net clinical consequences of consuming die- tary saturated fats by analysis of changes in circulating lipids and lipoproteins alone. Doing so requires human studies with determination of appropriate cardiovascular disease endpoints and a series of recent analyses of the literature have now questioned the long-standing thesis that increased consumption of saturated fats is readily translated into greater cardiovascular risk (Siri-Tarino et al., 2010a; Siri-Tarino et al., 2010b; Siri- Tarino et al., 2010c; Mozaffarian et al., 2010; Astrup et al., 2011; Siri-Tarino, 2011; Sanders, 2012; Lawrence, 2013). In fact, most of the recent assessments have failed to support a direct relationship.
What’s The Hidden Curriculum and How Does this Manifest?
The above is a problem because which family physicians are going to take the time to verify the data behind what’s said in the paper?
As I mentioned in my recent podcast with @MightyCasey (see: Healthcare Is HILARIOUS! June 7 2018 edition – TED EYTAN! | Mighty Casey on Patreon), I am going to verify because I have a desire to know and because I’m aware of a hidden curriculum. In the podcast I referred to my Virgo nature, which also ties in a little…
Noting, also, that on the AFP Journal web site, you have to actually perform an additional click for the references to appear – they are occluded by default.
The Hidden Curriculum in Nutrition
“Hidden Curriculum” as defined in Wikipedia:
A hidden curriculum is a side effect of an education, “[lessons] which are learned but not openly intended”[1] such as the transmission of norms, values, and beliefs conveyed in the classroom and the social environment.[2]Hidden curriculum – Wikipedia
The example above makes me ask the question – what are the forces/environmental cues in place that cause the example above to happen, on a fairly regular basis?
- The presence (yes presence) of nutrition education in a physician’s career. It’s not that they don’t get education. It’s what they’ve been getting. Let’s look through the pages of the New York State Medical Society journal, circa 1957:
There’s more here – browse through them and note not just conflicting information about nutrition, but/and also the path paved for pharmaceutical interventions for obesity.
It continues. Go to 1966, and see the same pattern.
- The USDA guidelines themselves, which trickle down into a million different visible and invisible influences in a physician’s practice.
This includes everything from performance metrics to specialty society guidelines. Ask any physician how their success is measured, you’ll likely find a connection back to these guidelines. What are some examples you see in your practice? Feel free to include in the comments…
Regardless of which dietary pattern is mentioned, they all have the same composition of macronutrients.

For the 2020 Guidelines, the door is being opened to reconsideration of these defaults.
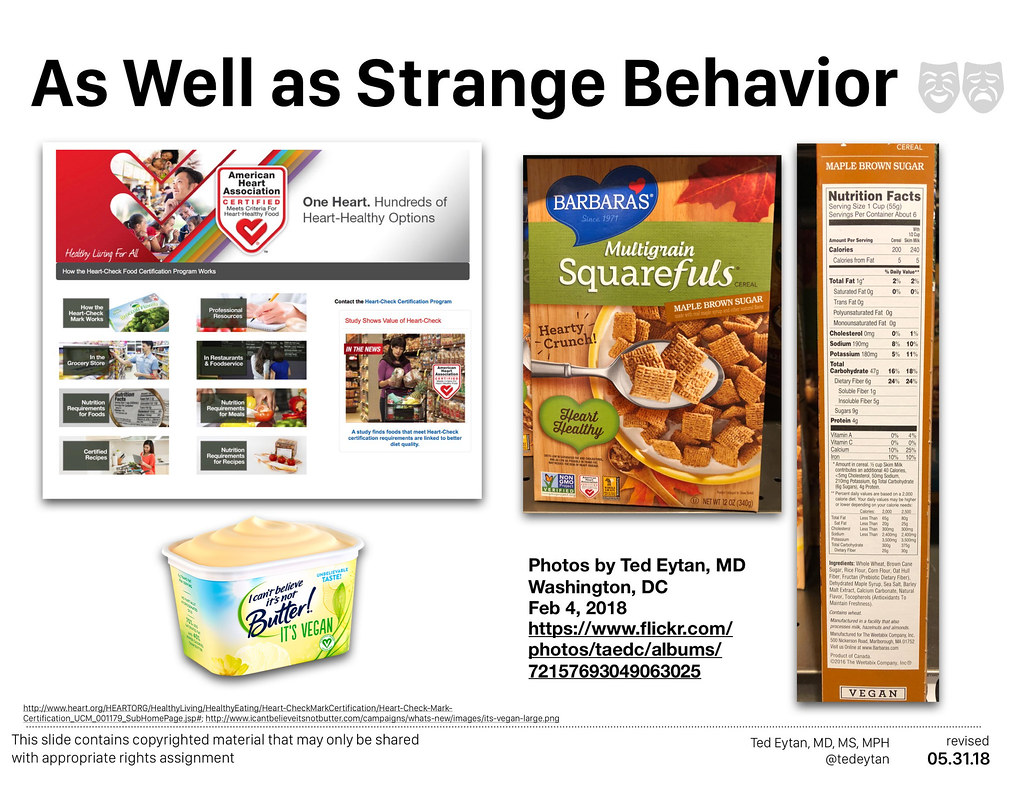
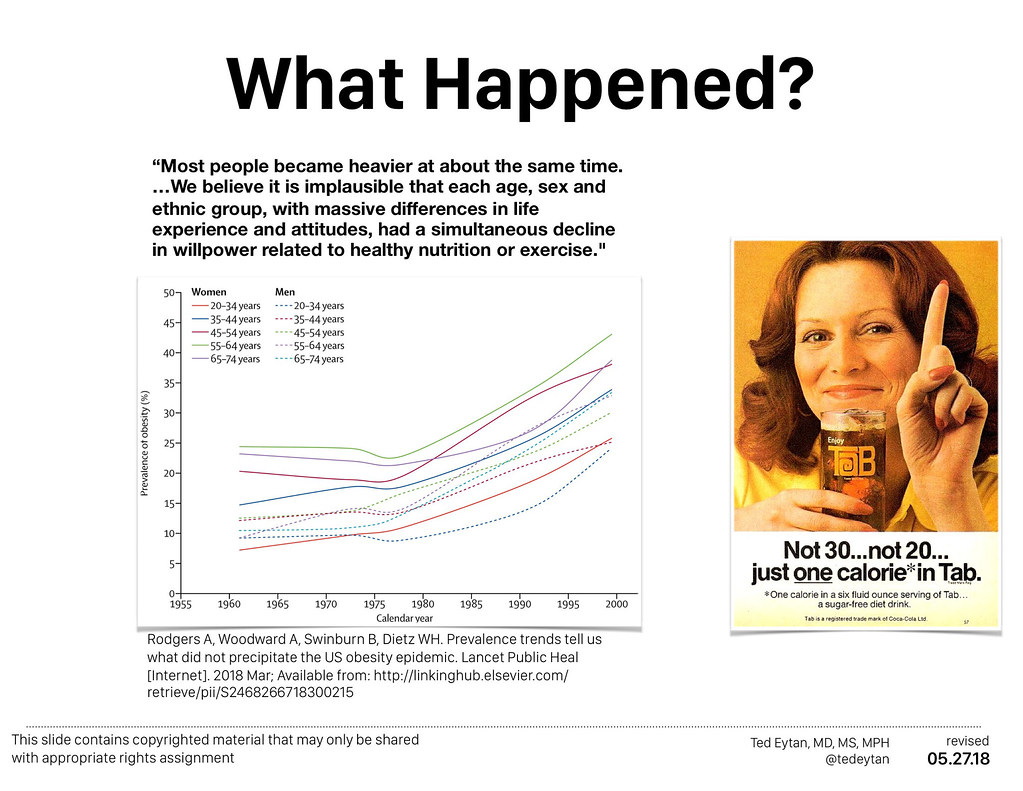
- The images and experiences in society that shape our biases – From my own deep dive of implict and explict bias (the connections to LGBTQ health are never very far), we know that physicians tend to have the same implicit and explicit biases as their surrounding communities – not more, not less.
We are confronted with ideas and images everywhere we go that make a statement about what the default is. And given the science that we now know, these defaults result in strange behavior.
The impact can be seen in the identified biases of medical students. Bias against obese people and LGBTQ humans are the last two accepted explicit biases in medicine:

“Heteronormative” and “Carbonormative”
This section in the Wikipedia entry on Hidden Curriculum:
The hidden curriculum of heteronormativity is the erasure of LGBTQ identities in the curriculum through the privileging of heterosexual identities.[7] Yep said, heteronormativity is the “presumption and assumption that all human experience is unquestionably and automatically heterosexual”Hidden curriculum – Wikipedia
I’ve lived a heteronormative world for the bulk of my professional career. It’s real, and still exists to a large extent. Because I’m aware of it, I manage around it. If one is not aware, which is the insidiousness of bias, there isn’t active management.
When I use the term “Carbonormative” I’d include carbon (as in carbon emissions) as well as carbohydrates. The former, we are learning in medicine, is a problem thanks to the work of organizations like Health Care Without Harm. Still, there is a tremendous lack of awareness of the impact of carbon emissions on human health.
We have a lot longer way to go with regard to carbohydrates, which is not to demonize them, it is to manage them as much as we are learning to manage our carbon exposure in the environment.
By the way, I have to point out that the two types of carbonormativity exist in separate worlds, as I was able to meet this breakfast (but not ingest it) at a recent event on the environment and health. Managing carbon but not carbohydrates:


“Although the hidden curriculum has negative connotations, it is not inherently negative”
Again, learning from the implicit bias literature, it is absolutely possible to to retrain our brains and modulate our conscious and unconscious responses to our environment. I’m doing that for myself by being diligent.
As I mentioned in the podcast, I do review the responses to peer reviewed literature both on journal websites, via Altmetrics which include social media coverage. There’s no other way to understand the literature anymore, especially with the subtle roadblocks in place (see @AFPJournal example above).
Our next steps are to
- Educate ourselves and colleagues about hidden curricula
- Expand what’s in the hidden curriculum while unhiding it
- Pursue the data, because it exists – #dataoverdogma
Why? Because this happened and it doesn’t have to continue 🙂 .
References cited
- American Academy of Family Physicians. A, Schneiderhan J, Zick SM. American family physician. Am Fam Physician [Internet]. American Academy of Family Physicians; 2018 Jun 1 [cited 2018 Jun 4];97(11):721–8. Available from: https://www.aafp.org/afp/2018/0601/p721.html
- Bier DM. Saturated Fats and Cardiovascular Disease: Interpretations Not as Simple as They Once Were. Crit Rev Food Sci Nutr [Internet]. Taylor & Francis; 2016 Sep 9 [cited 2018 Jun 9];56(12):1943–6. Available from: http://www.tandfonline.com/doi/full/10.1080/10408398.2014.998332
- Hunter JE, Zhang J, Kris-Etherton PM. Cardiovascular disease risk of dietary stearic acid compared with trans, other saturated, and unsaturated fatty acids: a systematic review. Am J Clin Nutr [Internet]. Oxford University Press; 2010 Jan 1 [cited 2018 Jun 9];91(1):46–63. Available from: https://academic.oup.com/ajcn/article/91/1/46/4597175
- Li Y, Hruby A, Bernstein AM, Ley SH, Wang DD, Chiuve SE, et al. Saturated Fats Compared With Unsaturated Fats and Sources of Carbohydrates in Relation to Risk of Coronary Heart Disease. J Am Coll Cardiol [Internet]. 2015 Oct 6 [cited 2018 Jun 9];66(14):1538–48. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26429077
- Zong G, Li Y, Wanders AJ, Alssema M, Zock PL, Willett WC, et al. Intake of individual saturated fatty acids and risk of coronary heart disease in US men and women: two prospective longitudinal cohort studies. BMJ [Internet]. British Medical Journal Publishing Group; 2016 Nov 23 [cited 2018 Jun 9];355:i5796. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27881409
- Phelan SM, Dovidio JF, Puhl RM, et al. Implicit and explicit weight bias in a national sample of 4,732 medical students: The medical student CHANGES study. Obesity (Silver Spring). 2014;22(4):1201–8. Available at: www.ncbi.nlm.nih.gov/pubmed/24375989 [Accessed April 2, 2014].