Deliberately avoiding the term “greening” as too much like “tree-hugging,” Dr. (David) Pencheon (head of NHS’s Sustainable Development Unit) argues that whole new models of care are needed, with new financial incentives that reward medical behaviour that benefits both human health and the environment. (Moynihan R. The greening of medicine. BMJ. 2012;344(jan16 1):d8360-d8360.)
#greenHC is a better hashtag – Meredith convinced me that shorter-but-clear wins every time. – ePatientDave (@ePatientDave) via Meredith Gould (@MeredithGould)
So, again, as in the last post (#greenhealthcare part 4: Health Information Technology helps health care be green), the support of a healthy environment that does not undermine/defeat what we are doing in the health care system is connected to how we enable and involve patients and families in their health and health care.
A big thanks to ePatientDave for the shiny new hashtag. He understands that these posts describe a leading edge concept for many in health care and wants to help me communicate it well. I’ll take all the help I can get!
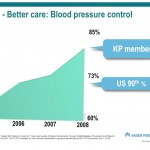
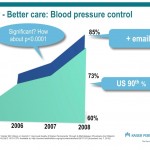
The slides above are meant to demonstrate a shift in the model of health care to make it more efficient – people who communicate electronically with their doctor are much more (significantly so) likely to have their blood pressure controlled, their blood sugar levels controlled (not pictured), their cholesterol lower (not pictured), and their eyes and kidneys checked for damage before they go blind or go on dialysis (not pictured) (See: Now Reading: Improved Quality At Kaiser Permanente Through E-Mail Between Physicians And Patients).
Performing preventive care OR treatment increase the CO2 footprint of health care, prevention more than treatment. This is okay, health care is supposed to be an investment in a longer, higher quality of life. In cardiovascular care, the one exception is smoking cessation, which is cost saving. Everything else costs money:
If all the recommended prevention activities were applied with 100% success, those costs would be reduced by $904 billion, or almost 10%. However, assuming the costs shown in Table 2, the prevention activities themselves would cost $8.5 trillion, offsetting the savings by a factor of almost 10 and increasing total medical costs by $7.6 trillion (162%).(Kahn R, Robertson RM, Smith R, Eddy D. The impact of prevention on reducing the burden of cardiovascular disease. Circulation. 2008;118(5):576-85
Almost any health care activity, then, generate CO2 (in the US, about 8% of the greenhouse gas footprint, in the UK, 3%). In the United States, 14% of the CO2 generated by health care activities come from prescription drugs. In the UK, it’s 22%. These may actually go up if all prevention activities were applied uniformly to the population, so the prevention part that saves CO2 comes from delivering these services more efficiently, or not requiring these services at all.
The “delivering more efficiently,” example is in the slides above. The not requiring these services at all comes from prevention of nutritionally related diseases. Just four of these (cancer, high blood pressure, diabetes, and heart disease) are estimated to account for 1/3 of the US health care carbon footprint, and the estimate is that half of these could be mitigated by dietary changes. By “mitigated” we mean not requiring any preventive care or treatment in the health care system.
This is extensively modeled in the white paper “Harvie J, Schettler T, Mikkelsen L, Flora C. Common Drivers Common Solutions. 2011.”
Next post in #greenHC – measurement, an advantage of understanding green house gas emissions in health care.
These blog posts are a series connected to an upcoming presentation at American College of Preventive Medicine 2012, on February 22, 2012. You can see the whole series here.