The quote in the title of this post is the paraphrase of a conversation I have had more than a few times with someone who has asked me, “Ted, what’s the return on investment for web services for patients?” The answer I have usually gotten when I ask the question back is usually no answer.
Two papers just published in HealthAffairs provide a little more background for that conversation. The first is about the growth of the use of imaging technology in the United States. As you might expect, it is growing, and more with every new scanner put in operation.
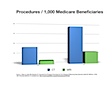
To put things in better perspective, I created this graph from the data, showing the increase in the number of scans/beneficiary. In 2005, there were 547 CT scans per 1,000 Medicare beneficiary, or about 1 scan per 2 beneficiaries. What the article doesn’t mention is that the radiation load from a CT scan is high, anywhere to 15 – 100 times the dose of radiation from a chest X-ray. Medicare reimburses, on average $308 for a CT scan, $713 for an MRI.
A basic return on investment analysis is performed for abdominal aortic aneurysm (AAA) screening, which shows that as more people are screened using CT, less are screened using catheter angiography (which is more invasive). This is good, except, the reduction is less than 1:1, so there is overall expansion of screening to more people, and more procedures to fix AAA associated with this. The problem is that there isn’t data on whether this is overall a good thing or not from a cost/benefit perspective.
Because CT and MRI are a physician preference item, reimbursement and use is typically physician directed, which can create conflict (see Jaime Robinson’s paper in the same Health Affairs issue for more about this).
It’s interesting that the adoption curve of CT/MRI looks a lot like the adoption curve of personal health records in organizations that prioritize them, like Kaiser Permanente and Group Health Cooperative.
Currently, Medicare pays $0.00 per certified empowered/activated patient (potentially defined by more than 2 accesses to a comprehensive personal health record in 6 months).
So we know from this is example that it’s possible for health care to adopt technology. How can we recreate the magic of the CT/MRI adoption curve for something that’s patient directed? I have some ideas but want to see your comments first.