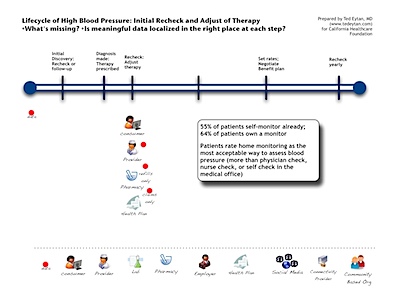
This is third of a multi-part series on a patient’s experience managing a chronic condition, in this case hypertension. A diagnosis has been made, and our patient is following up to see if the therapy is working or if adjustments need to be made.
Click on the image to see it larger size
Patient Story (Frydman)
I was supposed to go back but I didn’t do it. During a business trip I did try checking my BP with a home tool a few times and every time the BP was well within the norms, helping me be even more in denial. But then the next time I went to my friend’s office the data still showed clear HBP. Go figure!
(On the use of home monitors)It was first a few times on a specific day. Then a couple of times the next day. I then thought I would buy an OMRON blood pressure monitor. But I conveniently forgot about it when I returned to my home. No he (my doctor) didn’t say a thing about it. His behavior made me believe that he was not supportive of the home monitoring.
Clinical and Public Health pearls (Houston-Miller)
- Many patients already self-monitor (55 %, do it, 64 % own a monitor) – many have not been trained how to monitor correctly, and may over monitor; the most accurate way to monitor is twice per day, once in the morning, once in the evening, for 7 days. Patients should not monitor during the day and should not monitor while at work. These measures have not been shown to correlate with future organ damage as well as the morning and evening measures.
- The estimates of “masked hypertension,” or high blood pressure that appears normal in the doctor’s office are probably much greater than the 10 % reported; many patients restart medications in advance of coming to see their physicians (“similar to flossing your teeth a week before the dentist appointment”).
Comment
Where is the data? As in previous encounters, the data is again localized away from the patient and with the provider and ancillary services. Patients are asked to come back (physically) to the physician office to have their blood pressure rechecked and evaluated. The result is that the patient must ask for their blood pressure data from their provider, not the other way around.
What’s missing? If patients do not return in person (where their provider can bill for an office visit), there is no workflow in place in the majority of healthcare to assess blood pressure control, so these patients often go undertreated or untreated. Although 47 % of physicians recommend home-monitoring, many do not know recommendations for appropriate monitoring, including calibration of monitors, monitoring technique, and counseling on the value of home monitoring.
There is also a missed opportunity to leverage social networking, for connections to patients who may have recently been diagnoses and are integrating monitoring and treatment into their daily lives, similar to what occurs at the PatientsLIkeMe Community. Current data shows that there is a significant risk of being untreated or undertreated (4 – 11 times) among patients who have not seen a doctor in the past year. It’s as possible that these data are confounded by the fact that for most patients, management of the condition is stipulated by the care system to be an office-based activity.
Next post, a slight switching of gears to the annual health plan/employer interaction. Comments welcomed, of course